What are the survival statistics after a stent?
What they don’t tell you when you leave the hospital
Mortality statistics for everyone who gets a stent (for any reason):
1 in 50 (2%) die before leaving the hospital. (1)
4 and a half year death rate: about 1 of 10 (12%) die in 4.4 yrs. (from MI and from bleeding complications of blood thinners) (2)
1 in 20 die within 1 yr (from all causes): 4.6% (1)
1 in 10 die within 3 yrs (from all causes): 11% (1)
1 in 5 die within 5 yrs (from all causes): 18% (6.6% from heart attacks and 11% from everything else) (1)
After your first stent
Make sure you’re doing everything possible so you never need another one.
Ask the right questions, like “What’s causing the inflammation that caused my blockage?”
If you’ve just had your second stent or your second heart attack
Your prevention program is not working.
Why isn’t it working?
You have risk factors you don’t know about, risk factors that have not been identified or haven’t been adequately treated.
Unidentified and untreated risk factors cause arterial inflammation. Arterial inflammation makes plaque get worse. And it makes plaque dangerous.
Inflammation is the problem
Not blockage.
If blockage was the problem, then stents for blockage would save lives and prevent heart attacks, even without chest pain.
But they don’t. (3,4)
Severe blockage which obstructs the flow of blood causes chest pain. Stents are great for chest pain patients with severe blockage.
But in patients with no chest pain, stents don’t save lives or prevent heart attacks.
The COURAGE trial, published in 2007, showed that stents are no better than medication therapy at preventing heart attacks, sudden cardiac death, or hospitalization in patients who do not have chest pain (1). The ISCHEMIA trial (2) showed the same thing: without symptoms like chest pain, and without left main disease (which is rare), stents don’t save lives.
If stents don’t save lives, why are they used?
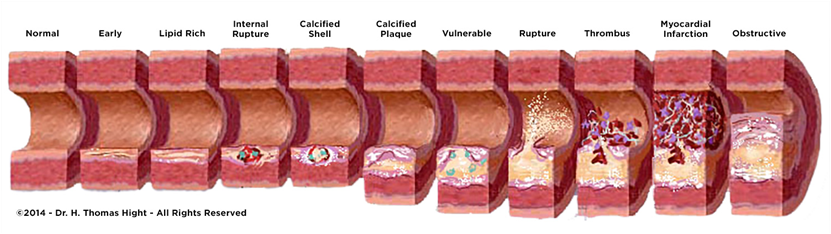
Stents and bypass procedures are useful to treat symptoms like angina, which is caused by obstructive plaque (see artery illustration below, far right).
Heart attacks happen when soft vulnerable plaque ruptures, which causes a clot, or a thrombus to form, which suddenly shuts off the blood flow to the heart muscle.
Most heart attack patients would have passed a stress test the day before.
Most heart attacks (86% or more) occur in people who, prior to the heart attack do not need a stent or bypass (see How Artery Disease Develops). (5,6)
Heart attack victims might get a stent after the heart attack has suddenly blocked off the artery. But most heart attacks are caused by vulnerable plaque, not obstructive blockage.
Most vulnerable plaque is not obstructive. And vulnerable plaque is much more common than obstructive plaque.
Angioplasty is a balloon placed inside the artery to smash open the obstructive plaque. A stent is a wire mesh tube placed into the artery to keep it open.
Fixing one small blockage doesn’t address the underlying forces that caused the blockage to develop.
Having a stent or bypass procedure means that your prevention program isn't working. Don't waste any more time. Find a prevention program that really works. Our works.
What to do after your stent?
Ask the right questions.
What caused the blockage?
Inflammation.
If each and every one of the underlying forces that caused the blockage to develop are not neutralized, the artery disease will only get worse. Fixing one little area of obstruction (or two or three) does not fix the underlying problems that caused the plaque to form and grow.
And your stent won’t prevent new plaque from growing. It won’t prevent the arterial inflammation getting worse. It won’t prevent the most dangerous type of plaque, soft vulnerable plaque, which ruptures and causes events (see the arterial illustration above).
Fix one blockage at a time?
Why just fix one small problem area at a time? Why not fix all the arteries, all over the body?
Aggressive medical therapy addresses the process that causes plaque to get worse, by addressing each and every risk factor. If all the arteries all over the body are getting better, no further stents or bypass will be needed.
And your risks for heart attack and stroke will be reduced.
why are stents more popular than prevention?
Click on the button below to watch a short trailer for the riveting film, The Widowmaker, from Patrick Forbes, the Director of Documentary Films at the BBC. You can buy the movie on Amazon.
how do you know whether you're getting better or worse?
Don't wait until you need another procedure. Don't wait to have an event.
A stress test can only tell you if you’re ready for your next stent. It can never predict who’ll have a heart attack because the stress test is designed to be normal when vulnerable plaque is present but no obstructive blockage.
By identifying soft vulnerable plaque and by trending plaque thickness, an ultrasound test can predict heart attacks and can tell you whether your arterial inflammation is getting better or worse over time. It costs about the same as a treadmill exercise test. And it’s a lot less expensive than a nuclear stress test. But it’s not covered by health insurance companies, which only pay for an ultrasound to measure blockage to flow, to answer whether you need a stent.
Compared to the carotid artery ultrasound (the standard one covered by insurance), our ultrasound measuring soft vulnerable plaque and plaque thickness is 10 x more powerful at predicting heart attacks and strokes! (7,8)
And our ultrasound checks more arteries than anyone. Come to Atlanta for trending once or twice a year. If your arteries are getting worse, you'll know it. Way before the stress test becomes abnormal. And you’ll be glad you came
Most people wait until they get another stent, or a heart attack. That’s the way they find out their prevention isn’t working. Some become statistics.
“I had my first stent at 40. Then I went 10 years without a problem. I had another stent at 50. When they put that second stent in, they didn’t see any other restrictions. No other problems at all. Eleven months later, they said I needed another stent put in for a 99% blockage. That concerned me. I asked the Cardiologist if there was anything else that could be done. He only kept me on Zocor. I wanted to find someone to help me from a prevention standpoint. It is important to me because I have a medical background. I wanted to know as much as I could about prevention. I was really impressed when I came to Atlanta for this testing. I believe people need two different specialists: someone who does a great job putting in stents, and someone who does a great job at prevention.”
references:
This study compares post-stent death rates among three different time periods. As stent technology and medications improved, the death rate from MI improved over time, but non-cardiac death rates increased (which included bleeding complications from blood thinners). Heart failure deaths did not improve over time. Daniel B. Spoon, et al. Trends in Cause of Death After Percutaneous Coronary Intervention. Circulation Volume 129, Issue 12, 25 March 2014; Pages 1286-1294
Best statistics for stent-related death risks are from this study with 32,900 stent patients on anti-platelet therapy, which combines death from heart attacks and from the bleeding complications of blood thinners after the stent: Dhruv S. Kazi, et al. Association of Spontaneous Bleeding and Myocardial Infarction With Long-Term Mortality After Percutaneous Coronary Intervention. J Am Coll Cardiol. 2015 Apr, 65 (14) 1411–1420
Both the COURAGE trial and the ISCHEMIA trial showed that stents don’t save lives or prevent heart attacks in patients with no chest pain, unless there is left main disease, which is rare. Although both the COURAGE and ISCHEMIA trials are important in re-shaping the way we think about coronary artery disease, they both describe large populations. Neither trial answered the question whether stents might save lives where obstructive lesions also contain soft vulnerable plaque seen on CT angiogram. And rarely, some people have “widowmaker” lesions in the left main artery, where surgical procedures do save lives. And some people have odd symptoms like diminishing exercise tolerance or jaw pain or fatigue. Not everyone has the typical symptoms of chest pain. So each patient must be individualized. Boden, William, et al. the COURAGE Trial Research Group, Optimal Medical Therapy with or without PCI for Stable Coronary Disease, N Engl J Med 2007; 356:1503-1516 DOI: 10.1056/NEJMoa070829
David J. Maron, et al. for the ISCHEMIA Research Group, Initial Invasive or Conservative Strategy for Stable Coronary Disease. N Engl J Med 2020; 382:1395-1407 DOI: 10.1056/NEJMoa1915922
Little WC, et al. Can coronary angiography predict the site of a subsequent myocardial infarction in patients with mild-to-moderate coronary artery disease? Circulation. 1988;78:1157-1166
Symptoms are treated with procedures like stents and bypass surgery when the degree of stenosis or obstruction is 70% or more. Yet 86% of heart attacks are caused by plaque lesions which are < 70% obstructed, and 68% of heart attacks are caused by lesions which cause a stenosis < 50%. E. Falk, PK Shah, V Fuster, Coronary Plaque Disruption, Circulation 1995;92:657
Iemolo F et al. Stroke 1/22/2004. Available at: http://stroke.ahajournals.org
Osamu Honda,MD et.al.; Journal of ACC, vol. 43, No. 7, 2004: 1177-1184