High Cholesterol
Where does cholesterol come from?
Cholesterol is a very important molecule. Lipids, also called lipoproteins (blood fats) transport energy from the gut to the liver and other body tissues. Cholesterol is used by the body as a building block for hormones like testosterone and estrogen. It is also used as a supporting structural element in cell walls. When cholesterol is too low, anemia, testosterone deficiency, and irregular periods can occur.
Cholesterol is produced in the liver and in other tissues and is also absorbed in the gut. Both production and absorption can be influenced by genetics. Liver production can be influenced by weight gain (which increases production) or weight loss (decreasing production) or by statin drugs, which block liver cholesterol production.
Dietary cholesterol sources like red meat (beef or pork) and eggs influence how much cholesterol is absorbed in the gut. Oatmeal works like a sponge, holding cholesterol in the gut, taking it through the system, thereby decreasing gut absorption. Some medications also block absorption.
What are the different types of cholesterol?
There are two types of cholesterol: the bad ones and the good ones. The bad ones cause artery disease. We call these the "atherogenic" lipids because they generate atherosclerosis. The total cholesterol number represents the total of the good and the bad types. The good cholesterol is HDL. All the others are bad. The best way to measure the bad cholesterol is called the Apo-B, a sum total of the bad ones. Apo-B predicts heart events better than LDL. Remember B stands for bad. Another way of measuring and thinking about the bad cholesterol is to subtract the HDL (the healthy cholesterol) from the total cholesterol, to give the "non-HDL cholesterol" value, which is a total of the bad ones, the atherogenic types of cholesterol.
Chylomicrons are absorbed from the gut, and then dismantled into smaller and smaller particles called triglyceride, IDL, VLDL and LDL. These are also known as "chylomicron remnants."
If you try to add up the different types on your lipid panel, that number may not equal the "total" cholesterol because there are other minor types not measured on a lipid panel. It is more useful to think about cholesterol as a combination of good and bad types. Apo-B is the total of all the bad ones, with all the chylomicron remnants (the triglyceride, IDL, VLDL and LDL). Apo-A1 is the good cholesterol.
The baddest of the bad:
Lipoprotein (a) is the worst possible type of bad cholesterol. It is doubly bad because LP(a) actively makes plaque worse by increasing inflammation. It also has a sticky cork-screw protein that increases risks for blood clots. If your LP(a) is high, you should discuss it with your doctor, or contact us. Although LP(a) is not often checked, it is one of the most dangerous risk factors.
What was your ldl before you started medications?
People with an untreated LDL of 190 or above have Familial Hypercholesterolemia which increases event risk by a factor of 10x. Most people who have familial hypercholesterolemia have not yet been diagnosed by their doctors.
how should ldl cholesterol be treated?
Losing weight lowers LDL by decreasing cholesterol production in the liver. Eating less cholesterol lowers absorption.
Numerous studies have shown that drug treatment to lower LDL reduces the risk of heart events. The problem is that in clinical trials, fixed statin doses were used, which failed to answer these questions: How much treatment is needed? Should treatment be based on LDL targets or on event risk? Compared to targeting LDL, targeted ApoB reduction is a more powerful predictor of risk reduction.
Are LDL sub-particles important?
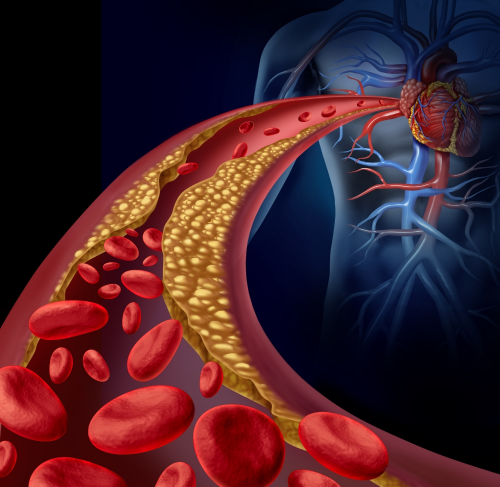
There are different types of LDL, called "LDL sub-particles." Big "fluffy" LDL molecules are not as dangerous as the little ones, called "small dense LDL," which are about the same size as the space between the cells lining the inside of the artery, called "endothelial cells." In the same way a marble might get stuck in the crack of a sidewalk, small dense LDL sub-particles can get inside the gap between the endothelial cells, becoming lodged underneath in the wall of the artery where they cause even more inflammation and plaque to develop. Over time, plaque builds up until soft vulnerable plaque ruptures, causing a clot to develop, forming a heart attack or a stroke.
Small dense LDL is associated with being overweight and with insulin resistance. LDL sub-particle sizes can be improved by weight loss and by drugs like niacin and fibrates (2). Although increased levels of small dense LDL is an independent risk factor for atherosclerosis (3,4), no randomized studies have proven that targeted treatment focused on shifting small dense LDL to larger LDL subparticle classes will lower the risk of heart events. But this may be one mechanism (in addition to others like insulin resistance) by which weight loss together with statin therapy seems to work better than statin therapy alone.
cholesterol not the only risk factor:
Although cholesterol is an important risk factor, 50% of heart attack victims have a normal cholesterol level (5).
Lp(a) is an especially dangerous type of LDL particle with a corkscrew-shaped protein attached to it. Lp(a) promotes development of artery disease and can cause increased absorption of cholesterol into the aortic valve, which can cause aortic valve stenosis. Due to similarities between the Lp(a) molecule and plasminogen (a protein involved in blood clotting), Lp(a) increases the risk of having blood clots. Blood clots inside the arteries cause strokes and heart attacks. So when high cholesterol is combined with high Lp(a), the risk of heart attack increases 3-4x.
triglycerides:
Whereas cholesterol is absorbed from animal fats, triglyceride is absorbed from the gut in the form of vegetable fats and milk fat. Additionally, blood sugar is converted into triglycerides. High triglyceride is associated with increased risk of heart disease. Some people are genetically predisposed to have extremely high triglyceride levels, which can cause pancreatitis.
Triglycerides can be lowered by reducing intake of sweets, vegetable fats and milk fat, and by losing weight. Medications can also lower triglyceride levels. Only about 3% of people who have high triglycerides are being treated (8).
HDL:
Thinking of the different types of cholesterol in terms of those that cause artery disease (the non-HDL cholesterol) and those that do not cause disease (the HDL) is a helpful way to think about cholesterol. But the danger is that if we focus too much on non-HDL cholesterol, we can overlook HDL related risk factors. Whereas LDL increases inflammation, HDL decreases inflammation by removing cholesterol from the diseased arteries, a process we call "reverse cholesterol transport." Because HDL works like an artery scrubber, we call it the "healthy" cholesterol.
One way to measure the good cholesterol particles is the Apo-A1. Remember, like A-1 steak sauce, A-1 is the good stuff. Apo-B is the bad cholesterol. The ratio of Apo-B to Apo-A1 is a way of comparing how much of the bad cholesterol you have, relative to the good stuff.
Raising low HDL levels lowers heart attack and stroke risk. For each 1 mg/dl increase in the HDL level, the risk of cardiovascular events drops by 2-3% (6).
Genetics can affect the quantity, quality and function of HDL.
are hdl sub-particles important?
There are different types of HDL, different sizes. The largest HDL sub-particles, loaded up with cholesterol esters to be transported out of the plaque, play an important role in removing cholesterol (7). Reverse cholesterol transport is an active energy-dependent process.
how can i raise a low hdl?
The best way to raise HDL is by exercising and losing weight. "Cardio" type exercise works best. Lipid-lowering medications can also raise HDL, lowering CV event risk (8). Statins and fibrates have a variable effect on HDL. When niacin (which raises HDL) was used in the setting of maximal LDL reduction, it was shown not to be beneficial in two large clinical trials using relatively low doses (9,10). Even though niacin at higher doses has been shown in a number of smaller studies to lower the risk of CV events (11, 12, 13, 14), it remains controversial. An article recently published by Dr. Robert Superko reviewed the current controversy and the body of evidence about HDL-focused niacin therapy (15).
Disclosure: Dr. Hight has a patent pending for a pharmaceutical combination to block the niacin flush.
references:
Stone NJ, et al 2013 ACC/AHA Guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129:S1-S45
Florentin M, et al. Effect of non-statin lipid lowering and anti-obesity drugs on LDL subfractions in patients with mixed dyslipidaemia. Curr Vasc Pharmacol. 2010 Nov;8(6):820-30.
Manjer J, et al. The Malmö Diet and Cancer Study: representativity, cancer incidence and mortality in participants and non-participants. Eur J Cancer Prev 2001;10:489-99.
Manjer J, et al. Invitation to a population-based cohort study: differences between subjects recruited using various strategies. Scand J Public Health 2002;30:103-12.
Sachdeva et al. Lipid levels in patients hospitalized with coronary artery disease: an analysis of 136,905 hospitalizations in Get With The Guidelines. Am Heart Journal. 2009;157(1):111-117.e2.
Gordon DJ, et al. High-density lipoprotein cholesterol and cardiovascular disease: four prospective American studies. Circulation. 1989;79(1):8-15.
Asztalos, et al. High-density lipoprotein subpopulation profile and coronary heart disease prevalence in male participants of the Framingham Offspring study. Arterioscler Thromb Vasc Biol 2004;24;2181-2187;DOI:10.1161/01.ATV.0000146325.937.a8
Grover S, et al. Evaluating the incremental benefits of raising high-density lipoprotein cholesterol levels during lipid therapy after adjustment for the reductions in other blood lipid levels. Arch Intern Med. 2009;169 (19): 1775-1780
The AIM-HIGH Investigators. Niacin in pateints with low HDL cholesterol levels receiving intensive statin therapy. N Engl J Med 2011;365:2255-67
The HPS2-THRIVE Collaborative Group, Effects of Extended-Release Niacin with Laropiprant in High-Risk Patients, N Engl J Med: 371:3, July 17, 2014, 203-212
Superko and King, et al. Lipid Management to Reduce Cardiovascular Risk: A New Strategy Is Required. Circulation, Jan 2008; 117: 560 - 568 (This is an excellent summary of the pre-AIM-HIGH/HPS2-THRIVE literature.)
Brown. Eur Heart J Suppl (October 2006) 8(suppl F): F60-F67. doi: 10.1093./eurheartj/sul043
Brown, et al Very intense lipid therapy with lovastatin, niacin, and colestipol for prevention of death and myocardial infarction: a 10-year Familial Atherosclerosis Treatment Study (FATS) followup. Circulation. 1998; 98 (supp I): 1-635.
Compared to the large clinical trials we've seen with statin drugs, smaller studies require a higher level of clinical change in order to achieve statistical significance. So smaller trials can actually reveal more dramatic clinical effects. We should not discount small trials which show highly significant results. In a paper (as yet unpublished) recently presented at the American College of Cardiology, authors Xue Qiao Zhao, Joseph Davis, Daniel Isquith, Alice Dowdy, Suzanne Boltz, Moni Neradilek, and B. Greg Brown reported a 20 year followup to the original FATs trial, where intensive care (niacin plus one or more LDL reducing agents) compared to usual care patients (LDL reduction alone) was associated with 71% reduction in CV mortality and a 66% reduction in all-cause mortality.
Superko, H.R., Niacin and heart disease prevention: Engraving its tombstone is a mistake. Journal of Clinical Lipidology. Nov-Dec 2017;11 (6) 1309-1317. https://doi.org/10.1016/j.jacl.2017.08.005